Category: Media
-
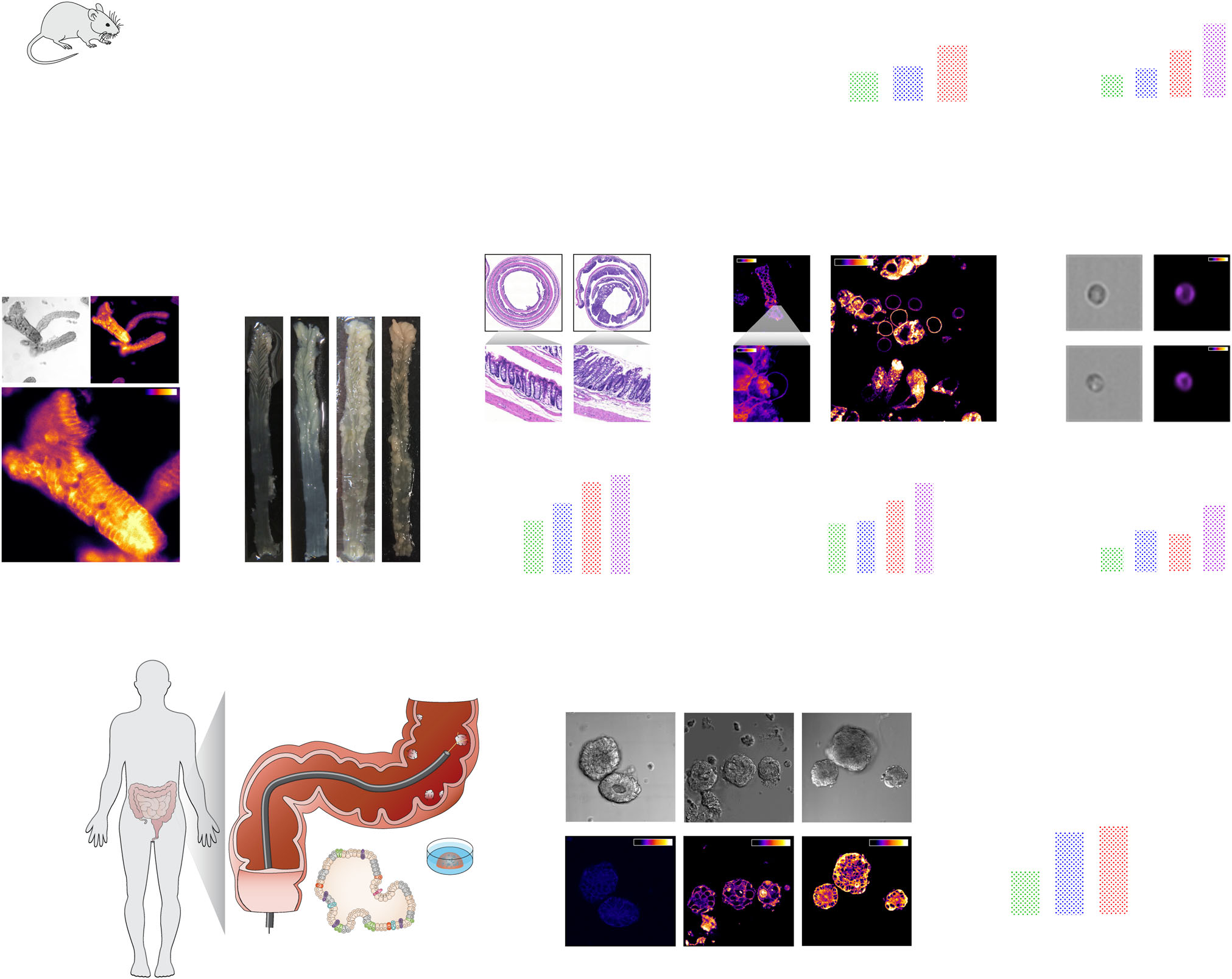
BREAKTHROUGH IN Wnt SIGNALING PUBLISHED!
Breakthrough publication! Our recent paper in Nature Communications explains the novel structure-function mechanism by which cholesterol promotes colon cancer. From a functional perspective, Wnt factors organize to form specialized plasma membrane (PM) domains. Dysregulation of Wnt domain structure can promote oncogenic Wnt signaling. Here, we describe an intricate Wnt signaling-associated mechanism involving oncogenic truncated APC…
-
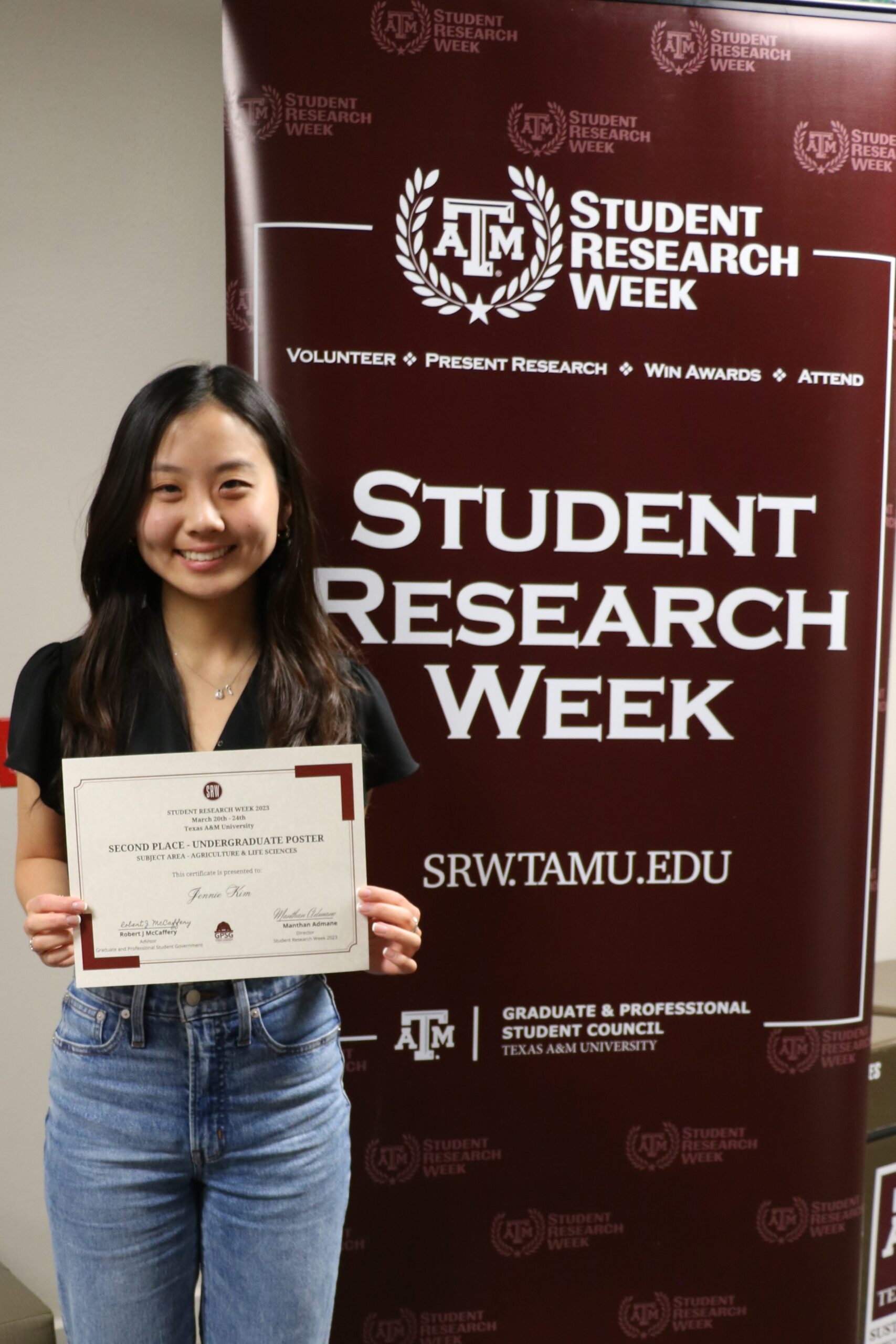
Chapkin Lab Undergrad Researcher Receives Award for Poster Presentation
Jennie P. Kim, a Nutritional Sciences major working on her Undergraduate Research Scholars Thesis in the Chapkin Lab (https://chapkinlab.tamu.edu) was recently awarded second place for her poster presentation in the Agricultural and Life Sciences category at the Texas A&M Student Research Week competition (https://srw.tamu.edu). Student Research Week is the largest student-run research symposium in the…
-
CPRIT – TREC GRANT FUNDED: Gene – environment – lifestyle interactions in cancer
The Chapkin Lab is pleased to announce the award of a $6 million grant from Cancer Prevention and Research Institute of Texas – TREC funding to support research in “Gene – environment – lifestyle interactions in cancer”. Dr. Robert Chapkin to serve as Deputy Director of the grant, Dr. Kenneth Ramos to serve as…
-
TEXAS A&M RESEARCHERS TO FURTHER DEVELOP UNIQUE CANCER DRUG WITH $2.3M NIH GRANT
Drs. Robert Chapkin, Gus Wright, James Cai, and Stephen Safe received a new NIH grant to perform a single cell multi-omic analysis of the colon tumor microenvironment to probe the mechanistic underpinnings of NR4A1-dependent modulation of T-cell exhaustion. Story by Jennifer Gauntt, VMBS Communications February 1, 2023 Preliminary data indicate that the compounds developed in…
-
Reappointed holder of the William W. Allen Chair in Nutrition & Chronic Disease Prevention in the Department of Nutrition
Congratulations! Dr. Robert S. Chapkin has been reappointed as the holder of the William W. Allen Chair in Nutrition & Chronic Disease Prevention in the Department of Nutrition for a second 5-year term from December 1, 2022 to November 30, 2027. As the holder of the William W. Allen Chair in Nutrition since December…